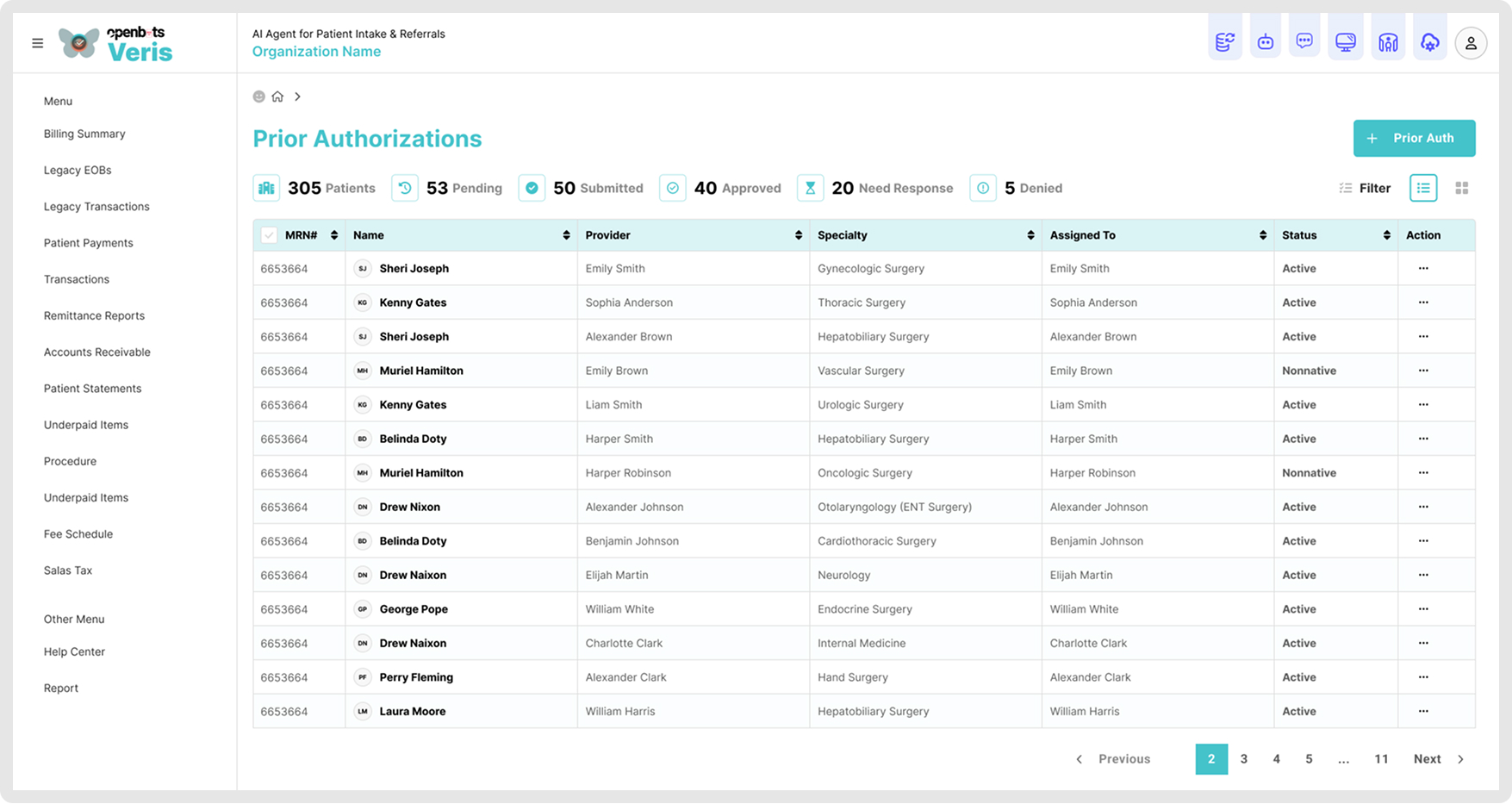
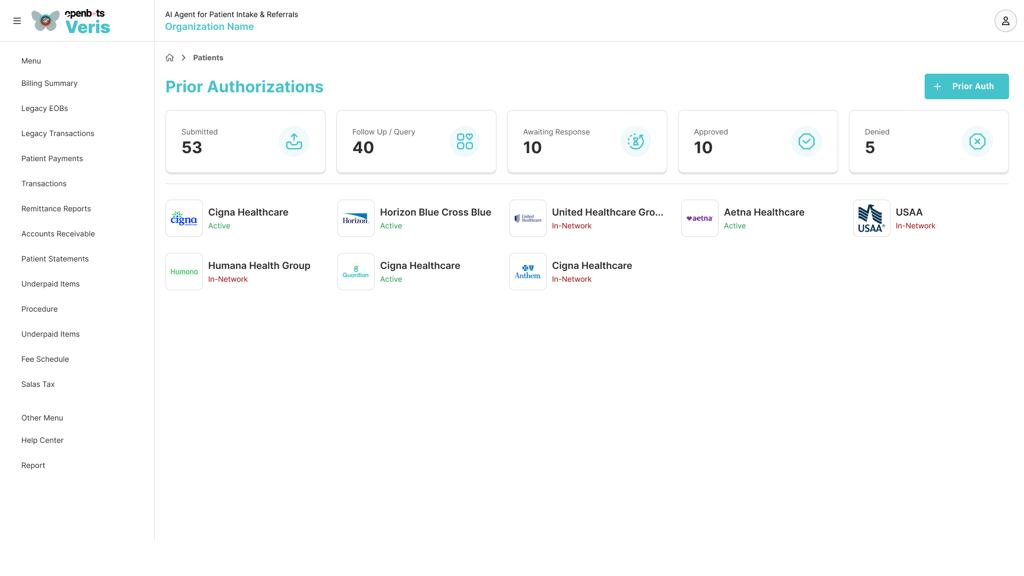
AI Agent for Insurance Verification & Prior Authorization
Streamline Insurance verification and Prior Authorization with our AI Agent designed for Autonomous execution
Trusted by
















From a technical requirements and scoping perspective, it’s been excellent working with the team. I appreciate how detail-oriented they are and how clearly they define what they want to achieve. Overall, it’s been such a positive experience working with OpenBots!


Clario has completely transformed our charge capture process. Missed charges have dropped significantly, and the accuracy of our coding has never been higher.

Compliance & Audit Lead (Riverstone Clinics)

Since implementing Clario, our revenue cycle team spends less time chasing down providers and more time optimizing workflows. The AI suggestions are spot-on.

Chief Medical Officer (Sunrise Health Group)
Copyright © 2026 OpenBots All rights reserved.
Security | Terms & Conditions | Privacy Policy | Do Not Sell My Personal Information| Status
We use cookies to ensure that we give you the best experience on our website. We also use cookies to ensure we show you advertising that is relevant you. You can change your cookie settings at any time. Cookies Policy | I accept